hypermobility exercises pdf

hypermobility exercises pdf
Hypermobile Spectrum Disorder (HSD) and Ehlers-Danlos Syndrome (EDS) are conditions affecting joint stability and movement․ Both involve connective tissue dysfunction, leading to joint hypermobility, musculoskeletal pain, and other systemic symptoms․ EDS is a genetic collagen disorder, while HSD is characterized by excessive joint movement without meeting full EDS criteria․ Proper exercise and management strategies are essential for improving quality of life and reducing complications in both conditions․

Understanding Joint Hypermobility and Its Implications
Joint hypermobility refers to excessive movement in joints beyond normal ranges, often linked to connective tissue disorders like HSD and EDS․ It can lead to musculoskeletal pain, instability, and increased risk of injuries․ While some individuals experience few symptoms, others may develop chronic pain or systemic issues․ Proper management involves tailored exercise programs to enhance joint stability and reduce discomfort․ Understanding the implications of hypermobility is crucial for developing safe and effective strategies to improve quality of life and prevent complications․
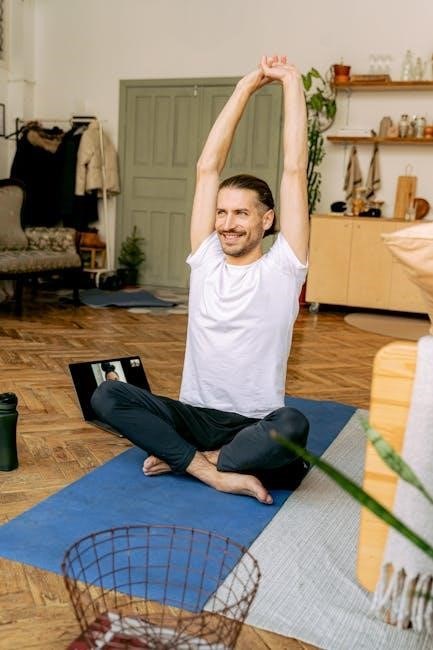
The Role of Exercise in Managing Hypermobile Conditions
Exercise plays a vital role in managing hypermobile conditions like HSD and EDS, helping to improve joint stability, reduce pain, and enhance overall function․ Gentle, controlled movements strengthen surrounding muscles, providing essential support to joints․ Activities like Pilates, yoga, and swimming are often recommended for their low-impact nature․ Proper warm-up and cool-down routines are crucial to prevent injury․ Exercise should be tailored to individual needs, focusing on stability and strength without overextending joints․ A personalized approach ensures safety and effectiveness in improving mobility and quality of life․
Safe Exercise Selection for Hypermobile Individuals
Safe exercise selection for hypermobile individuals focuses on low-impact activities that strengthen muscles without overextending joints․ Gentle movements, core stabilization, and controlled stretches are prioritized to enhance stability and reduce injury risk․

Low-Impact Activities and Their Benefits
Low-impact exercises, such as swimming, cycling, and Pilates, are ideal for hypermobile individuals․ These activities strengthen muscles and improve joint stability without excessive strain․ Swimming provides buoyancy, reducing joint stress, while cycling enhances cardiovascular health․ Pilates focuses on core strength and body awareness, promoting controlled movements․ Gentle yoga and tai chi can also improve flexibility and balance․ These activities help maintain mobility, reduce pain, and prevent injuries, making them essential for managing hypermobility effectively and safely․
Importance of Warm-Up and Cool-Down Routines
A proper warm-up prepares the body for exercise by increasing blood flow and reducing stiffness․ For hypermobile individuals, dynamic stretches and light cardio are ideal․ Cool-down routines, including gentle stretches and foam rolling, help prevent muscle soreness and promote recovery․ These practices reduce the risk of injury and improve joint stability․ Incorporating breathing techniques during warm-up and cool-down enhances relaxation and body awareness, making these routines essential for safe and effective exercise management in hypermobility conditions․
Strengthening Exercises for Joint Stability
Strengthening exercises are crucial for joint stability in hypermobile individuals․ Low-impact activities like core and lower extremity workouts enhance muscle support, reducing joint strain and improving mobility safely․
Core and Lower Extremity Strengthening Techniques
Core and lower extremity strengthening is essential for hypermobile individuals to enhance joint stability․ Gentle exercises like bridges, planks, and resistance bands target key muscle groups without overstraining joints․ Starting with controlled movements and progressing slowly ensures safety and effectiveness; Strengthening the core improves posture and reduces instability, while lower extremity exercises promote better alignment and support for joints․ These techniques are foundational for managing hypermobility and preventing injuries, fostering long-term mobility and strength․
Progressive Resistance Training Methods
Progressive resistance training involves gradually increasing exercise intensity to build muscle strength and support joints․ For hypermobile individuals, this can include gentle resistance bands or light weights․ Starting with low resistance and slowly progressing helps avoid joint strain․ Focus on controlled movements to enhance muscle support without overloading joints․ Regular monitoring ensures exercises remain safe and effective, promoting stability and reducing injury risk․ This approach is particularly beneficial for improving joint health in HSD and EDS, fostering long-term strength and mobility․
Pilates and Its Application in Hypermobile Conditions
Pilates is beneficial for hypermobile individuals, focusing on controlled movements and core engagement to enhance joint stability and body awareness․ Modified techniques ensure safe practice․
Pre-Pilates Approach for Safe Practice

A pre-Pilates approach is essential for hypermobile individuals to build foundational strength and stability before advancing to traditional Pilates exercises․ This method focuses on gentle, controlled movements to enhance body awareness and core engagement without overloading joints․ Techniques include breathing exercises, pelvic floor activation, and slow, precise movements to improve proprioception․ By starting with modified exercises, individuals can gradually progress, reducing the risk of injury and ensuring a safe transition into more dynamic Pilates routines tailored to their needs and limitations․

Focus on Breath and Body Awareness
Breath and body awareness are foundational in managing hypermobile conditions․ Deep breathing enhances core stability and reduces joint stress, while mindfulness improves movement control․ Gentle exercises, such as diaphragmatic breathing, promote relaxation and alignment․ Body awareness helps individuals recognize and avoid excessive joint movement, preventing overextension․ This mindful approach fosters a connection between breath and movement, ensuring exercises are performed safely and effectively, which is crucial for hypermobile individuals to maintain joint health and avoid injury․

Avoiding High-Impact and Harmful Exercises
High-impact exercises can exacerbate joint instability and pain in hypermobile individuals․ Avoid activities involving heavy weights, contact sports, and excessive stretching․ Opt for low-impact alternatives like swimming or cycling, which promote joint stability without overloading․ Always prioritize controlled movements and consult a healthcare professional to tailor exercises safely․
Why Certain Exercises May Worsen Symptoms
Certain exercises can worsen symptoms in hypermobile individuals by overstretching joints and destabilizing connective tissues․ High-impact activities, heavy weightlifting, and repetitive movements may lead to joint pain and inflammation․ Overextending joints beyond their safe range can cause micro-injuries, exacerbating instability and discomfort․ Additionally, exercises requiring extreme flexibility or rapid movements may strain already compromised tissues, making symptoms like joint subluxations and musculoskeletal pain more pronounced․ It’s crucial to avoid such exercises to prevent further complications and promote long-term joint health․
Alternatives to High-Risk Activities
For hypermobile individuals, low-impact exercises like swimming, yoga, and Pilates are excellent alternatives to high-risk activities․ These options promote strength, flexibility, and joint stability without excessive strain․ Cycling and gentle stretching can also be beneficial, focusing on controlled movements․ Activities that emphasize core engagement and proprioception are particularly advantageous, as they enhance joint support without overextending․ These alternatives help maintain physical fitness while minimizing the risk of injury or symptom exacerbation, making them ideal for long-term management of hypermobile conditions․

Managing Symptoms Through Exercise

Targeted exercises enhance joint stability, reduce discomfort, and improve functional movement in hypermobile individuals․ Strengthening muscles around joints and improving proprioception are key to symptom management and preventing further issues․
Improving Proprioception and Balance
Enhancing proprioception and balance is crucial for hypermobile individuals to reduce joint instability․ Simple exercises like single-leg stands, heel-to-toe walking, and balance board work can improve awareness․ Controlled movements, such as bridging or core exercises, strengthen stabilizer muscles․ These practices enhance neuromuscular feedback, reducing the risk of injury․ Gradual progression and focus on proper form ensure safety and effectiveness․ Improved balance and proprioception lead to better overall stability, reducing symptoms and enhancing daily functionality for those with hypermobile conditions․
Exercises to Enhance Muscle Support for Joints
Targeted exercises can strengthen the muscles surrounding joints, providing stability and reducing hypermobility-related discomfort․ Gentle movements like leg raises, bridges, and wall slides are effective․ Resistance bands or light weights can enhance muscle engagement without overstraining․ Controlled, low-impact exercises improve joint alignment and reduce excessive movement․ Strengthening the core and peripheral muscles creates a protective framework, minimizing joint stress and promoting functional mobility․ Consistency in these exercises is key to long-term joint support and stability for hypermobile individuals․

Genetic and Collagen Disorders Related to Hypermobility
Hypermobility often links to genetic collagen disorders like Ehlers-Danlos Syndrome (EDS), affecting connective tissue․ Collagen defects impair joint stability, causing excessive movement and systemic symptoms, requiring tailored management strategies․
Diagnosis Criteria for EDS and HSD
Diagnosis of Ehlers-Danlos Syndrome (EDS) and Hypermobile Spectrum Disorder (HSD) involves clinical evaluation of joint hypermobility, skin features, and family history․ EDS is confirmed by genetic testing for collagen defects, while HSD is diagnosed based on excessive joint movement without meeting full EDS criteria․ Both conditions require a multidisciplinary approach for accurate assessment and management, often involving geneticists and physical therapists to address systemic symptoms and improve quality of life effectively․
Impact of Collagen Structure on Joint Health
Collagen plays a critical role in joint stability and health․ In conditions like EDS and HSD, collagen defects lead to weakened connective tissues, causing joint hypermobility and instability․ This structural compromise can result in frequent dislocations, musculoskeletal pain, and chronic inflammation․ Strengthening exercises and physical therapy are essential to improve joint support and mitigate the effects of collagen-related deficiencies, enhancing overall mobility and reducing the risk of further complications in individuals with these conditions․
Lifestyle Balance and Exercise Routine
A well-balanced lifestyle and consistent exercise routine are crucial for managing hypermobile conditions․ Personalized plans, incorporating low-impact activities and strength training, promote stability and overall well-being while minimizing risks․
Creating a Personalized Exercise Plan
Creating a personalized exercise plan for hypermobile individuals involves consulting healthcare providers to tailor activities to specific needs․ Setting realistic goals, incorporating low-impact exercises, and prioritizing joint stability are essential․ Strength training, core work, and gentle stretching should be included, avoiding high-risk movements․ Progression should be gradual, with regular assessments to ensure safety and effectiveness․ This approach helps maximize benefits while minimizing injury risks, promoting long-term well-being and functional independence․
Monitoring Progress and Adjusting Routines
Regularly monitoring exercise progress and adjusting routines is crucial for hypermobile individuals․ Track improvements in strength, flexibility, and pain levels, ensuring exercises remain safe and effective․ Adjustments should be based on symptom feedback and physical changes, avoiding overexertion․ Consulting with healthcare providers or physiotherapists ensures personalized modifications․ This adaptive approach helps maintain joint stability, prevents injuries, and promotes long-term well-being, balancing activity with safety to support optimal health outcomes for individuals with hypermobility spectrum disorder or Ehlers-Danlos Syndrome․
Safe exercises and tailored routines are vital for managing hypermobility․ Consult resources like Mayo Clinic’s EDS guide and hypermobility exercise PDFs for comprehensive support and expert advice․
Final Thoughts on Safe and Effective Exercise
Safe and effective exercise is crucial for managing hypermobility, focusing on strengthening, flexibility, and stability without overloading joints․ Personalized plans, avoiding high-impact activities, and incorporating techniques like Pilates can enhance joint support and reduce discomfort․ Consistency and gradual progression are key to long-term benefits․ Consulting healthcare providers ensures tailored approaches, optimizing outcomes for individuals with HSD or EDS․ Regular monitoring and adjustments help maintain joint health and overall well-being, promoting an active, pain-managed lifestyle․
PDF Resources and Expert Recommendations
PDF resources and expert recommendations provide valuable insights into managing hypermobility through exercise․ Systematic reviews highlight the effectiveness of therapeutic exercises for joint stability and pain reduction․ Mayo Clinic and specialized EDS/HSD clinics offer comprehensive guides and exercise programs tailored to individual needs․ These resources emphasize the importance of personalized plans, gradual progression, and professional guidance․ They also recommend avoiding high-impact activities and focusing on low-risk exercises that promote joint support and overall well-being․ Consulting healthcare providers ensures safe and effective exercise routines․